Understanding the New Acuity Modifier Payments for FHOs
INTRODUCTION:
Effective April 1st 2024, FHO and FHN doctors will receive payment based on the complexity of their enrolled patients.
- It is worth the time to do the OMA’s self-directed course here.
- Plus, you get CME credits.
- It includes background references (downloadable PDFs)
- The OMA’s FAQ page is here, which also answers many common questions.
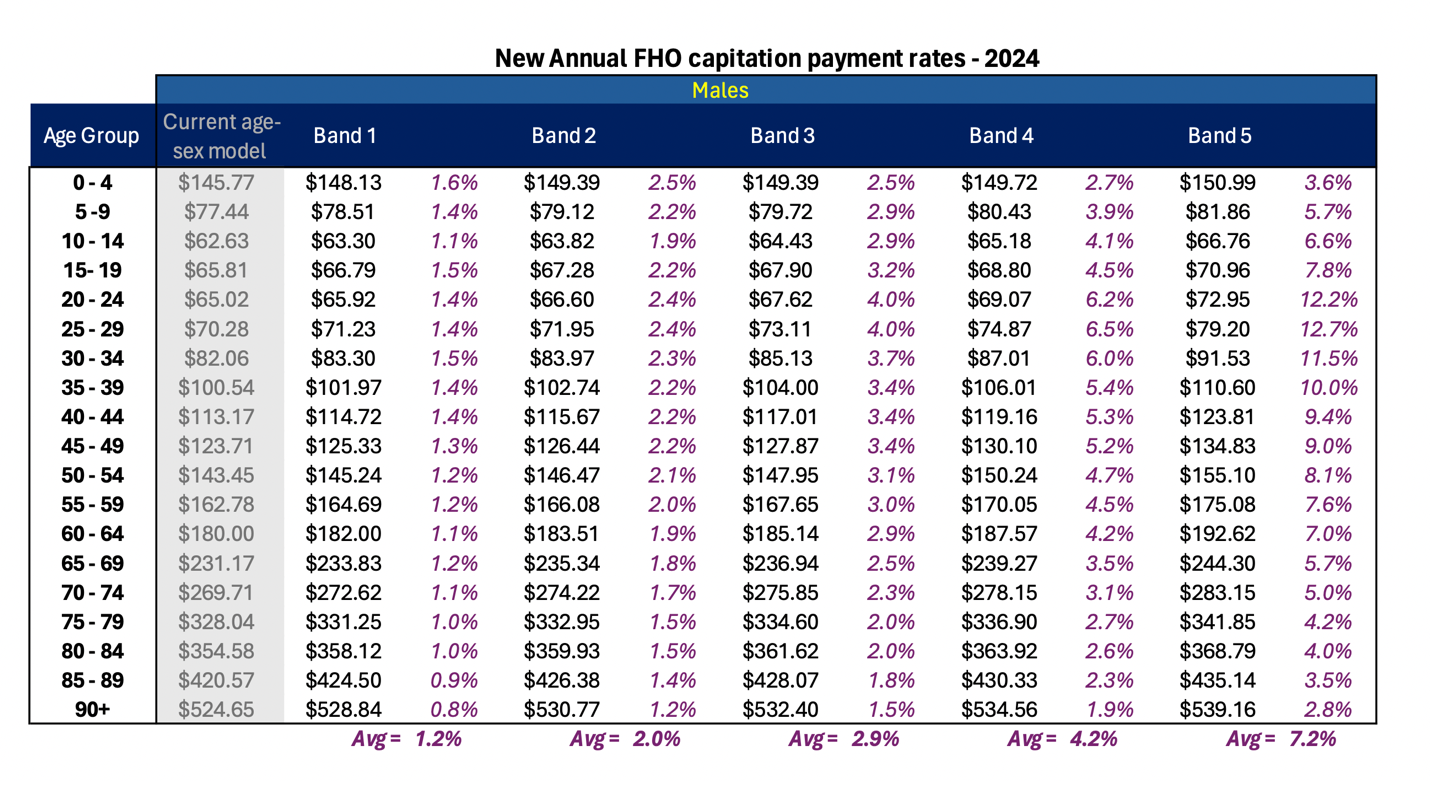
THE NEW CAPITATION PAYMENTS AND BANDS:
Here are the official tables are from the OMA’s page.
I further analyzed the numbers in spreadsheets:
MALES:
FEMALES:
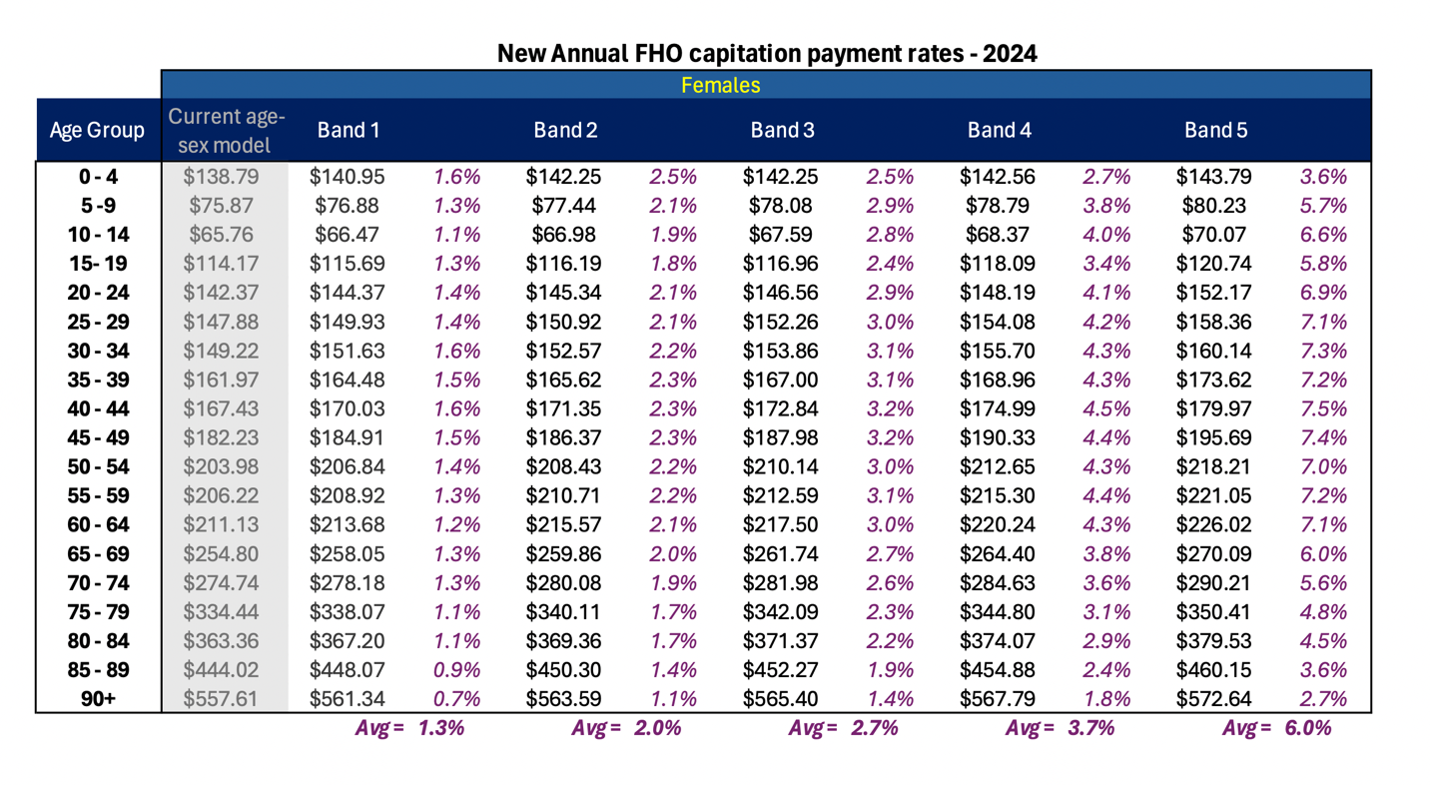
The overall average increase is 3.3%
CIHI’s Population Grouping Methodology:
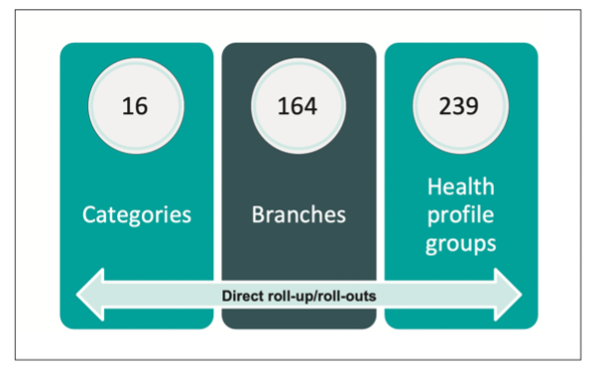
If you read the all the reference materials in the OMA’s self-directed course, there is a document that summarizes “CIHI’s Population Grouping Methodology 1.4”.
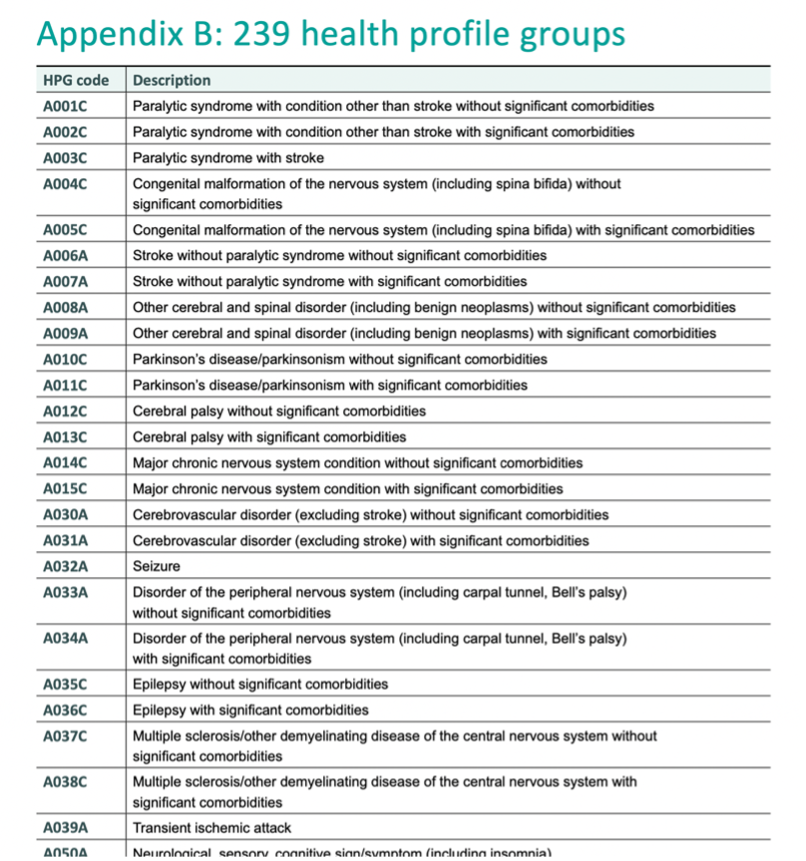
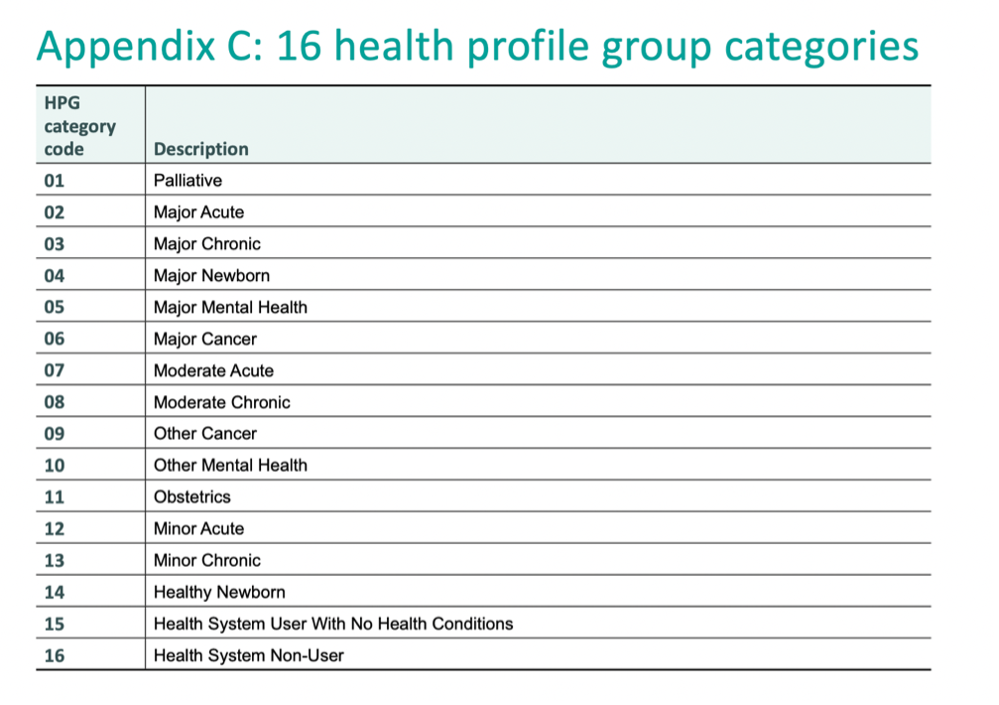
You will see summaries for different “Categories” and “Branches” and “Health Profile Groups”:
HOW DO ICD9 DIAGNOSTIC CODES GET MAPPED TO COMPLEXITY BANDS?
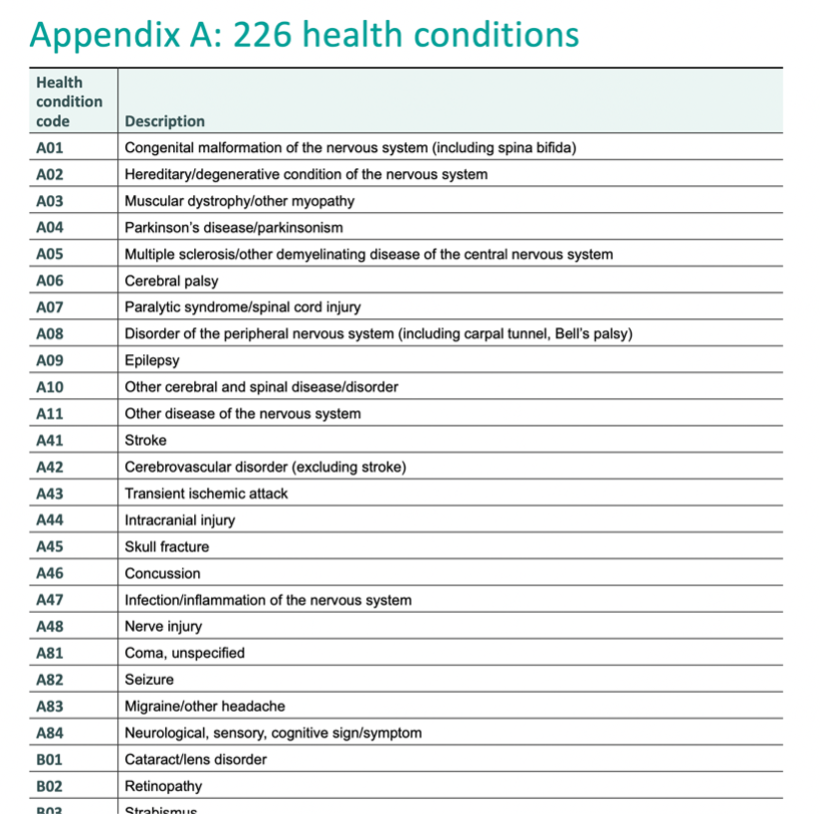
There is a master summary of how the ICD9 diagnostic codes get mapped.
- However, it is CIHI’s proprietary property and will not be shared.
- Plus, it’s not as simple as an algorithm for just ICD9 codes. The mapping is also affected by other overriding variables.
- There’s also all the hospital codes, specialist billings, and all the other data inputs to consider.
Ultimately, there are so many variables to consider that there are 5.7 million different permutations!
- It is not as simple as saying “Patients with Diabetes are put into Band 2”, or “Patients with Diabetes and Anxiety and Cancer go into Band 4.”
- It’s also not as simple as saying Anxiety is more complex than Hypertension, for example.
- Rather, there are 5.7 million different possibilities.
If you then listed all 5.7 million permutations from most complex down to least complex, and then split that list into quintiles (20% each), that is how patients land in a particular band.
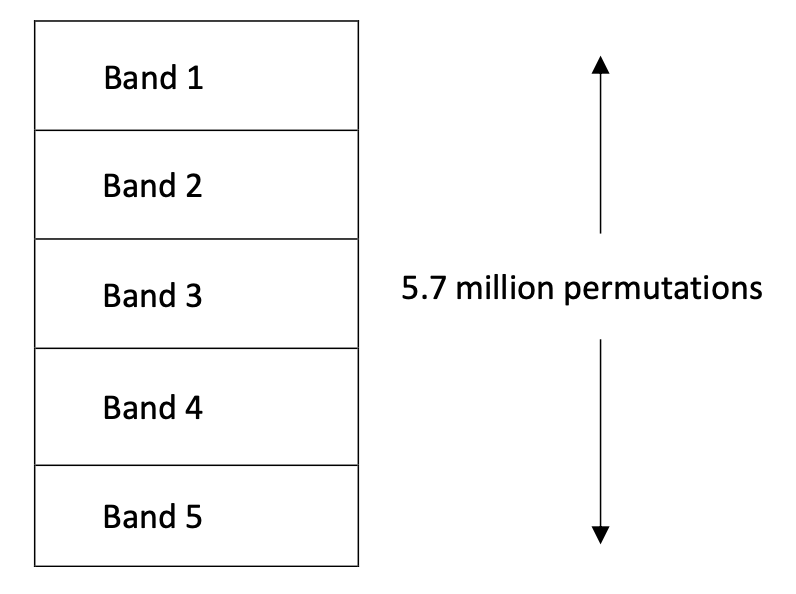
So, each band has over 1 million different possible “complexities” too.
Which is why it’s impossible to be as simple as “Diabetic patients are in Band 3”, for example.
WHAT TIMEFRAME OF BILLING DATA IS BEING USED?
The billing data looks back:
- 5 years for chronic conditions (i.e. mental health, cancer, diabetes)
- 2 years for acute conditions (i.e. URTIs, UTIs, stiches)
DOES VISIT FREQUENCY AFFECT THE BANDS?
Key point: NO
- Billing K030 vs A007 vs K005 does NOT affect which band to which a patient is ultimately assigned.
DOES THE SERVICE CODE AFFECT THE BANDS?
Key point: NO
- Visit frequency will NOT place a patient into one band versus another.
- You can still practice with multi-issue visits and that will not ‘reduce’ the patient’s assigned complexity.
A SPECIAL CONSIDERATION WITH DIABETES K030 BILLINGS:
K030 does NOT necessarily need to be billed with diagnostic code “250”.
- Family doctors need to bill a diagnostic code TWICE for the patient to be officially assigned that condition in the algorithm.
- So, you will want to make sure you bill “250” with a K030 at least TWICE every few years in order to have Diabetes accurately assigned to the patient.
- BUT, if you do multi-issue visits along with your diabetes visits, you will also periodically want to mix in some of the patient’s other diagnostic codes in order to better define that patient’s complexity.
DOES ROSTER SIZE AFFECT THE NEW ACUITY PAYMENTS?
Key point: NO
Many people misunderstood this.
All roster sizes, including those less than 1000 patients, will all receive the new acuity payments.
The confusion stemmed from the following:
- The preventative care bonuses for Child Immunizations and Flu Shots remain intact! (It is just the PAP, Mammo, and FIT bonuses that are ending).
- But for practices with rosters under 1000 patients, those bonus amounts would be pro-rated based on roster size.
- For example, if a FHO practice was only 500 patients, instead of receiving a $2000 bonus payment, it would be pro-rated to only $1000 (50%).
- The rationale is that smaller practices would require proportionally less work to reach the bonus thresholds.
- The money to fund the acuity modifiers had to be repurposed from somewhere.
WHAT OFFICIAL ICD9 CODE LIST SHOULD WE USE?
You will find variability in different ICD9 code databases.
** Here is the official MOH list of ICD9 codes. **
i.e. Our EMR databases sometimes differ from the OMA app or other ICD9 databases.
Our hope is that either I or SGFP will officially update and release an ICD9 list and/or tools.
OVERALL SUMMARY:
– by Dr. Adam Stewart
April 5th, 2024
