Family Medicine is a Dumping Ground for Other People’s Work
If you’re a Family Doctor, you’ll undoubtedly recognize all these expressions. And dozens more like them.
If you’re a Specialist, perhaps you’ve written or dictated phrases like these?
A System in Crisis
It’s no secret that our entire health system is in crisis. Its foundation, Family Medicine, is crumbling. Look no further than your daily newsfeed over the past several months. Every week there multiple headlines about the nearly 2 million Ontarians without a Family Doctor. And about how Family Doctors are leaving or retiring, so it’s only going to get worse.
Scariest of all, despite the recovery and resurgence since the 1990s, Family Medicine is again becoming less and less appealing. Fewer medical students are choosing to go into family medicine. The costs of running a Family Medicine Clinic are enormous.
There’s a colossal amount of administrative burden in Family Medicine. Some of it comes with the territory. But a significant portion of work falls upon the shoulders of Family Doctors because others deflect it there.
Family Medicine is dumping ground for others’ scut work. And it needs to stop.
It’s a Two-Way Street
Admittedly, this article contains some finger-pointing.
Just the same, we Family Doctors must also look in the mirror. We have an obligation to provide high quality care and collegiality to our specialist colleagues.
Also, none of this is meant to paint broad strokes. Many Specialists are fantastic. They follow patients comprehensively and never offload work. Accordingly, I suspect that many will be surprised to hear the common occurrences to follow.
I’ll come back to this at the end, but I first wanted to acknowledge the matter so it doesn’t pose as a distracting elephant in the room throughout.
A Review of the Schedule of Benefits
The Ontario Schedule of Benefits is explicit on many points.
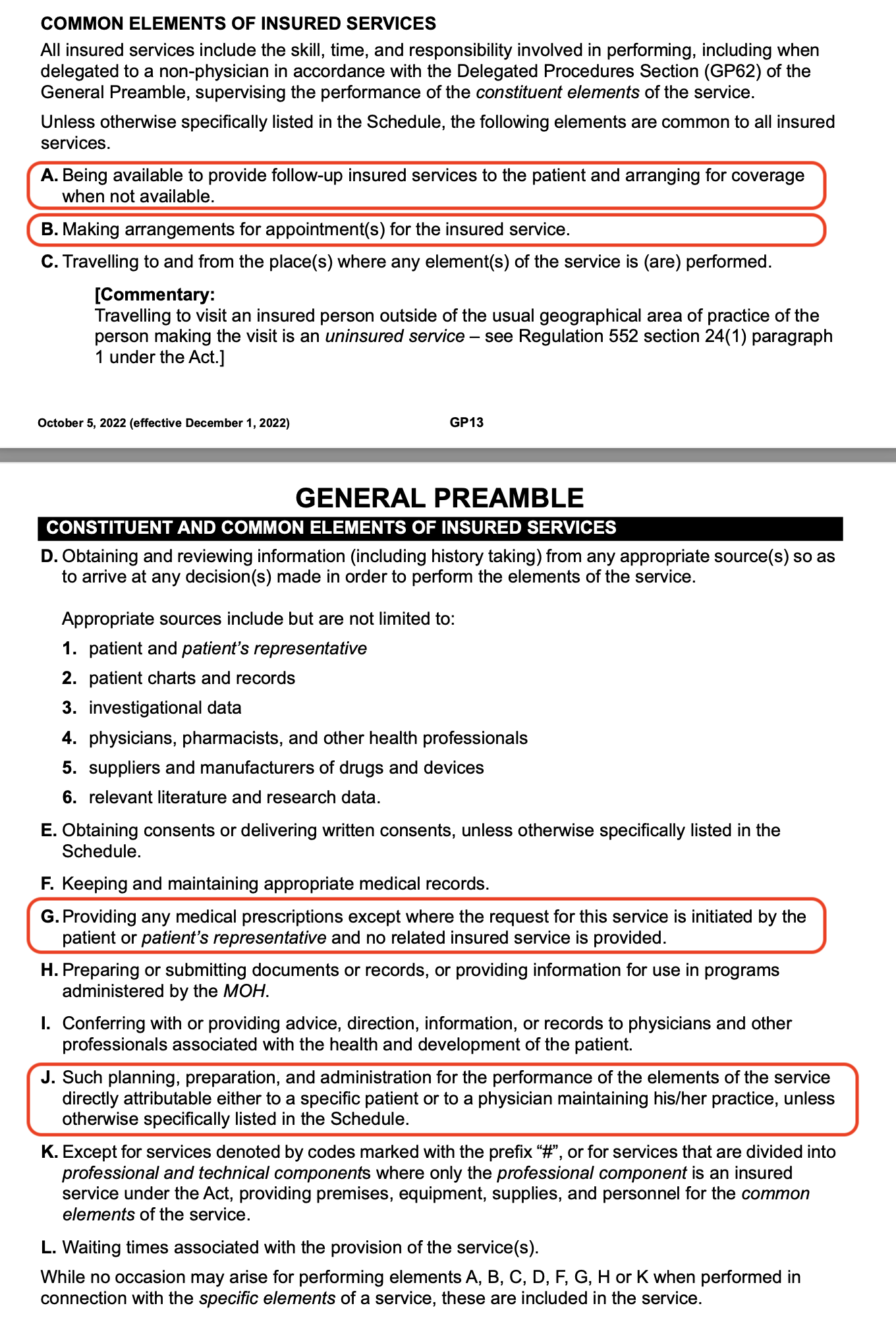
First of all, the Schedule of Benefits clearly states the Common Elements and obligations that are included under any fee code that a physician bills. See General Preamble Pages 13-14:
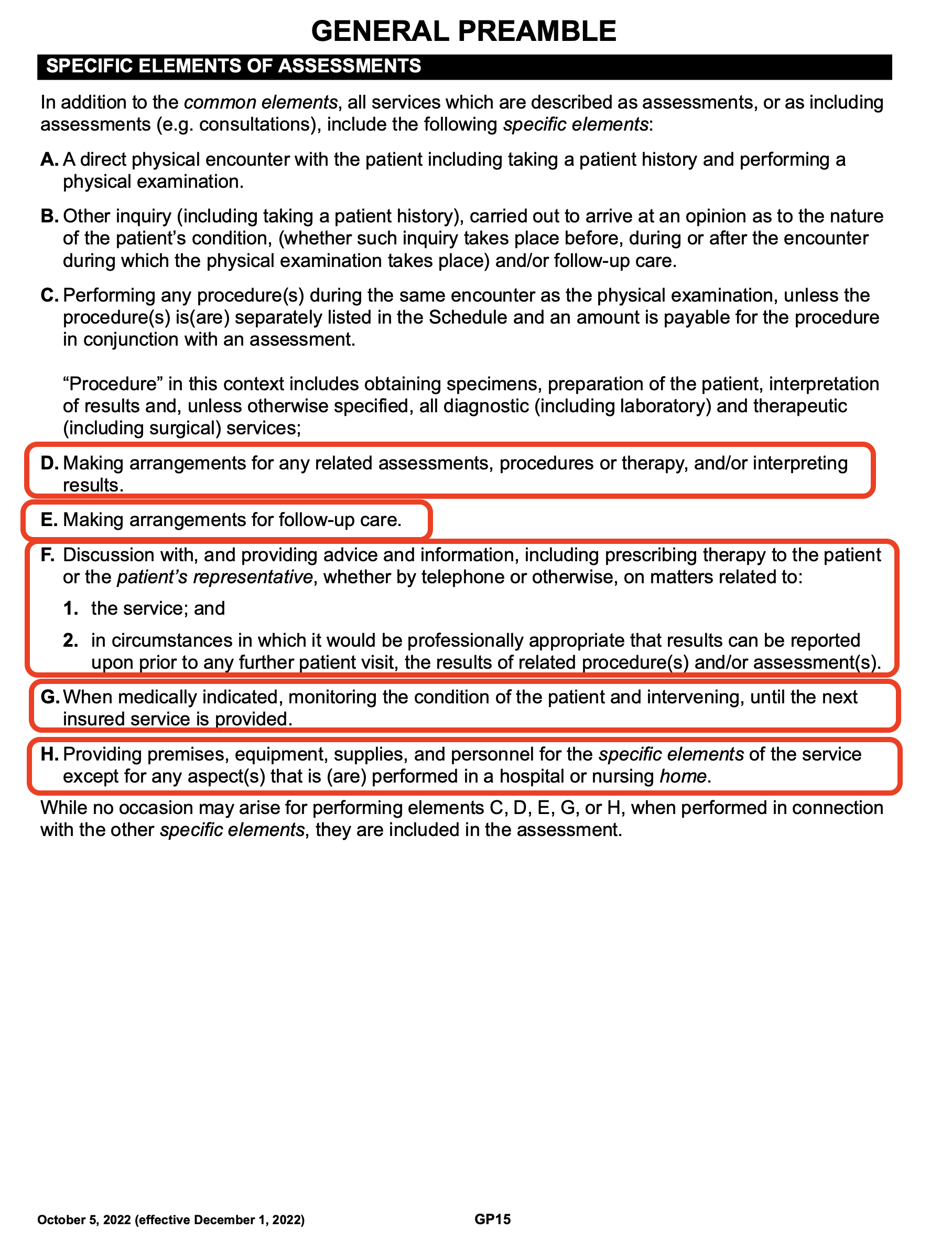
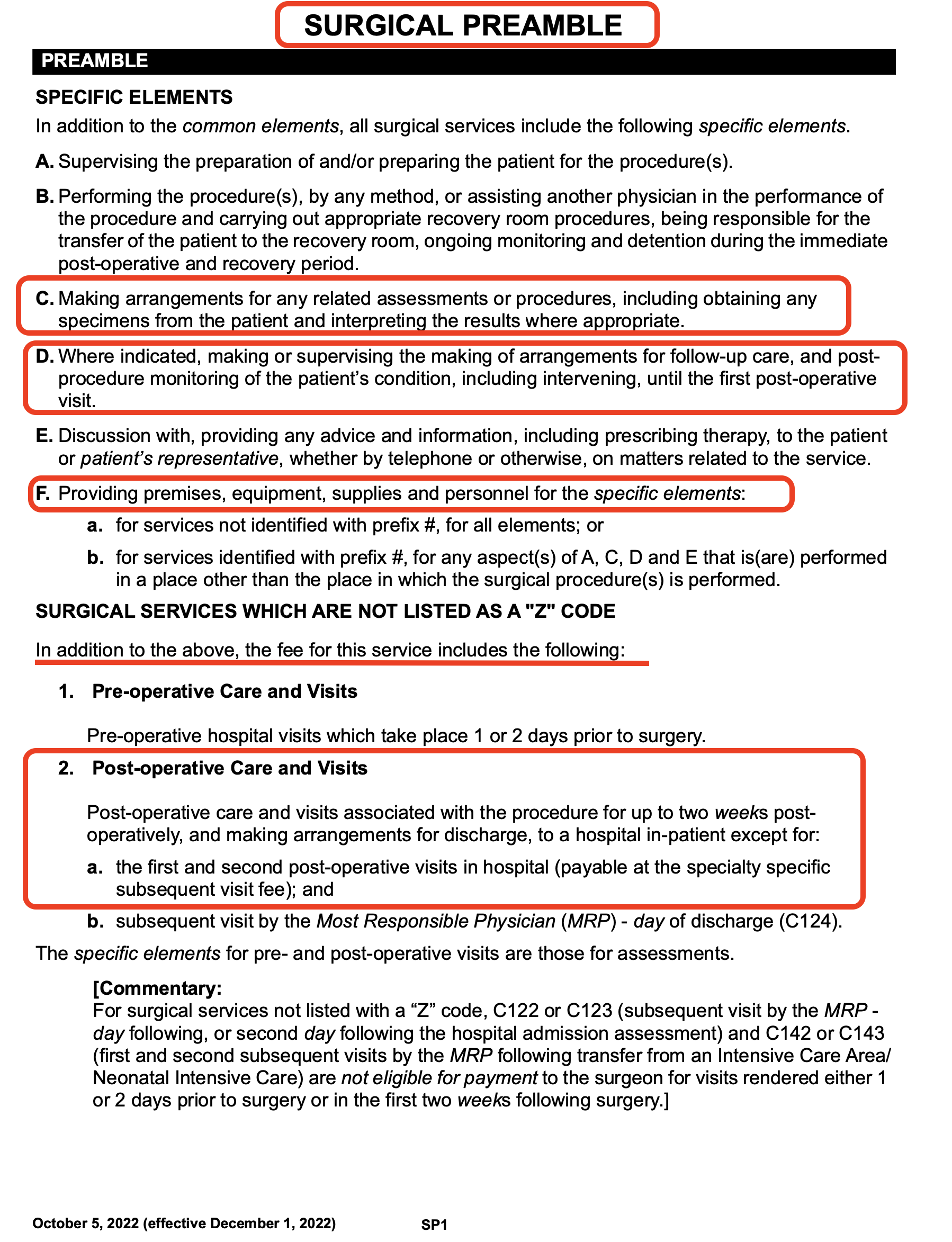
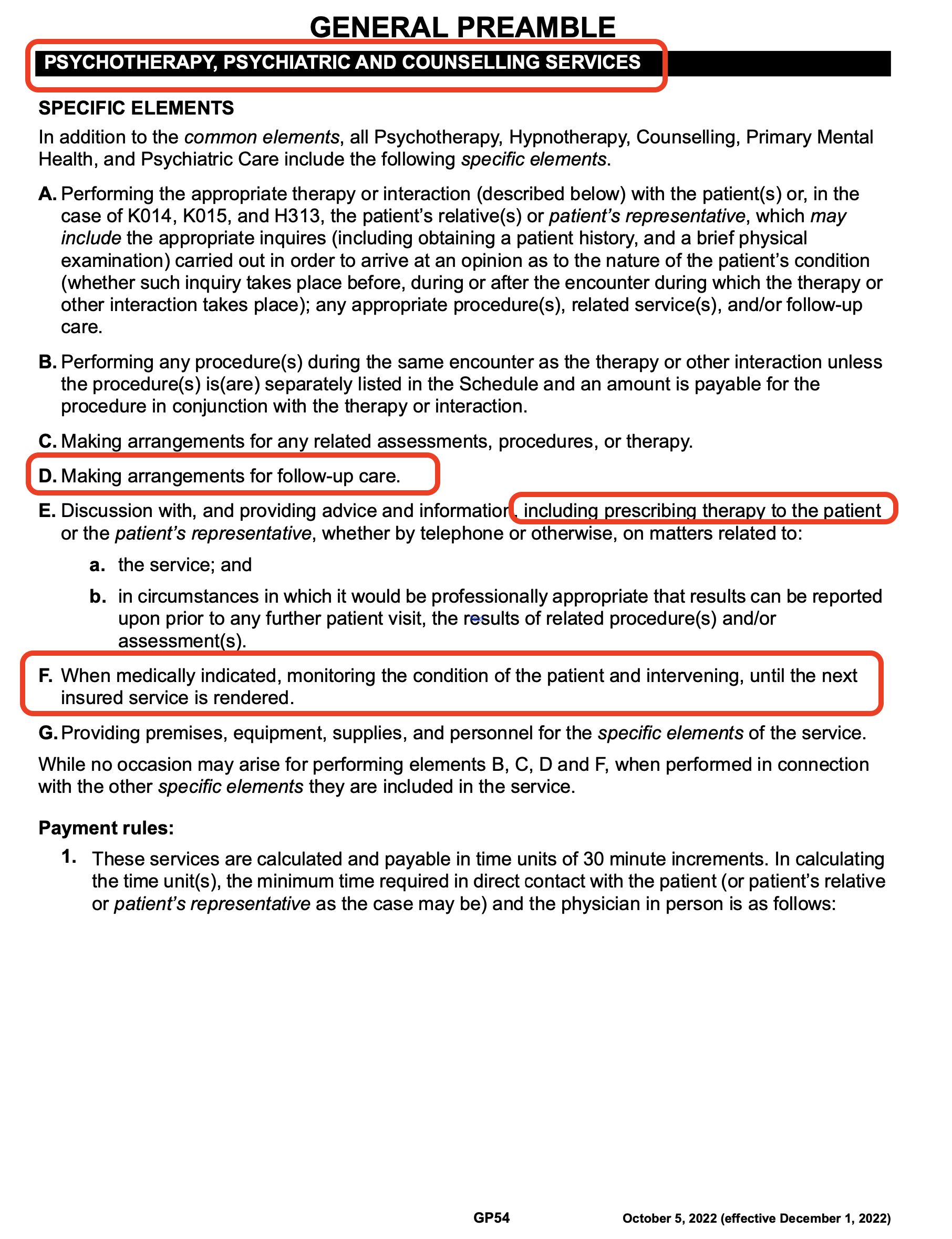
Furthermore, the Schedule of Benefits clearly states Specific Elements and obligations that are also included in fee codes.
Whether it be for Assessment Fee Codes (General Preamble Page 15):
Or Surgical Fee Codes (Surgical Preamble Page 1):
Or even Psychology and Counselling Fee Codes (General Preamble Page 54):
The point is, when a Specialist provides a service to a patient and bills OHIP for the corresponding fee code, that includes an obligation to fulfill all of the requirements.
So, thinking back to the opening of this article, how/why/when did any of these phrases become acceptable?:
Neurosurgeon Asks Family Doctor to Order CT Head:
A neurosurgeon performed a surgical procedure on one of my patients. I received the consult note that stated this:
Not even a “please” or “thank you”?
This administrative work is actually included in the surgeon’s fee code that he already billed OHIP.
But never mind that for a second. Is it not most medically appropriate for the surgeon to be the one who complete the CT requisition for the specific type of CT protocol and with the specific diagnostic questions? (That’s a rhetorical question).
It is in the patient’s best interest for the specialist to order (and interpret) their own tests.
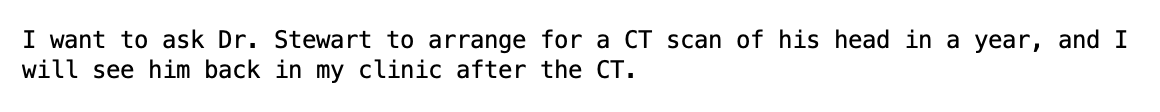
And by the way, here is the menu of options that we Family Doctors face when we need to order a CT head at our local hospital:
It is not within my scope nor expertise to be guessing which of these options the neurosurgeon requires.
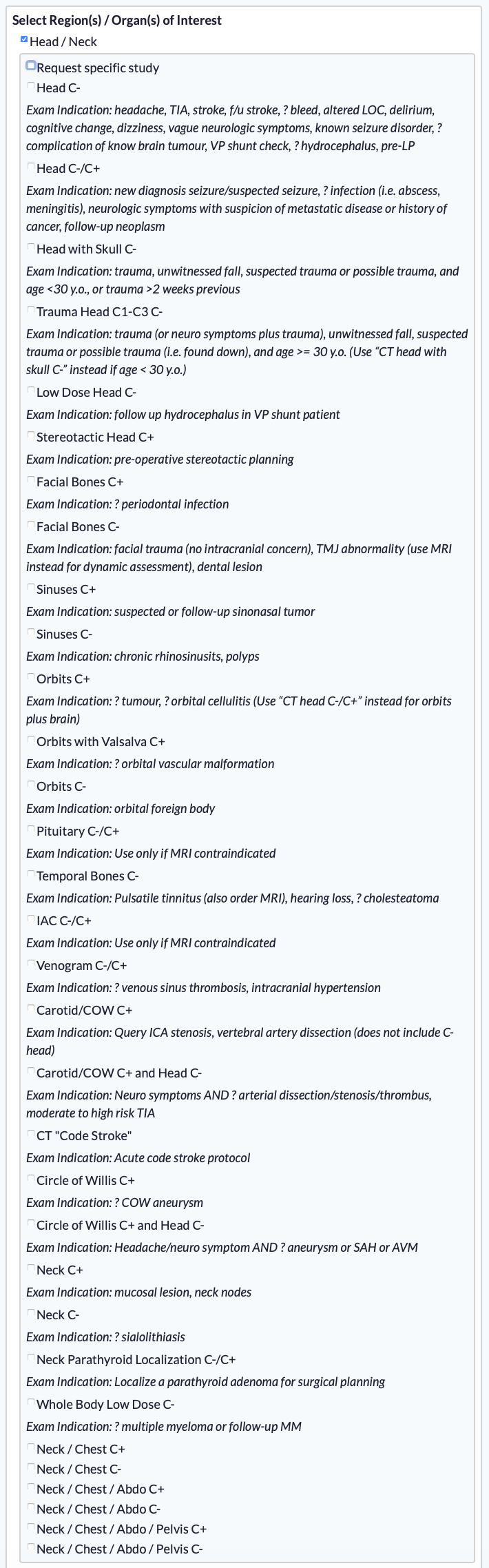
Now, back to the main point of Family Medicine being dumping ground for others’ scut work. Let’s look at the cost and resource burden to Family Doctor’s for requests like this:
Remember, all of this work is supposed to be included in the assessment and surgical OHIP fee codes that the surgeon has already billed.
Yet, these costs are being downloaded to the Family Doctor.
And what is worse, the Family Doctor does not earn a single cent of revenue for complying with requests like these. The Family Doctor is not able to bill OHIP any fee codes for this work.
It’s completely unacceptable.
Surgeons Ask Family Doctor to Remove Sutures
It is all too common for surgeons to advise patients to “follow up with your family doctor to have your sutures removed”.
Again, let’s set aside the associated costs for a second. Is it not in the patient’s best interest to follow up with their surgeon after a procedure, including for wound assessment? (Again, rhetorical). After all, it is the surgeon who has the expertise to know what to should be expected post-operatively, and what complications to watch out for.
Related to this, it’s equally common for a patient to be advised “follow up with your family doctor in two weeks” after a procedure. Why? Isn’t the person who performed the procedure the most appropriate person to reassess the patient?
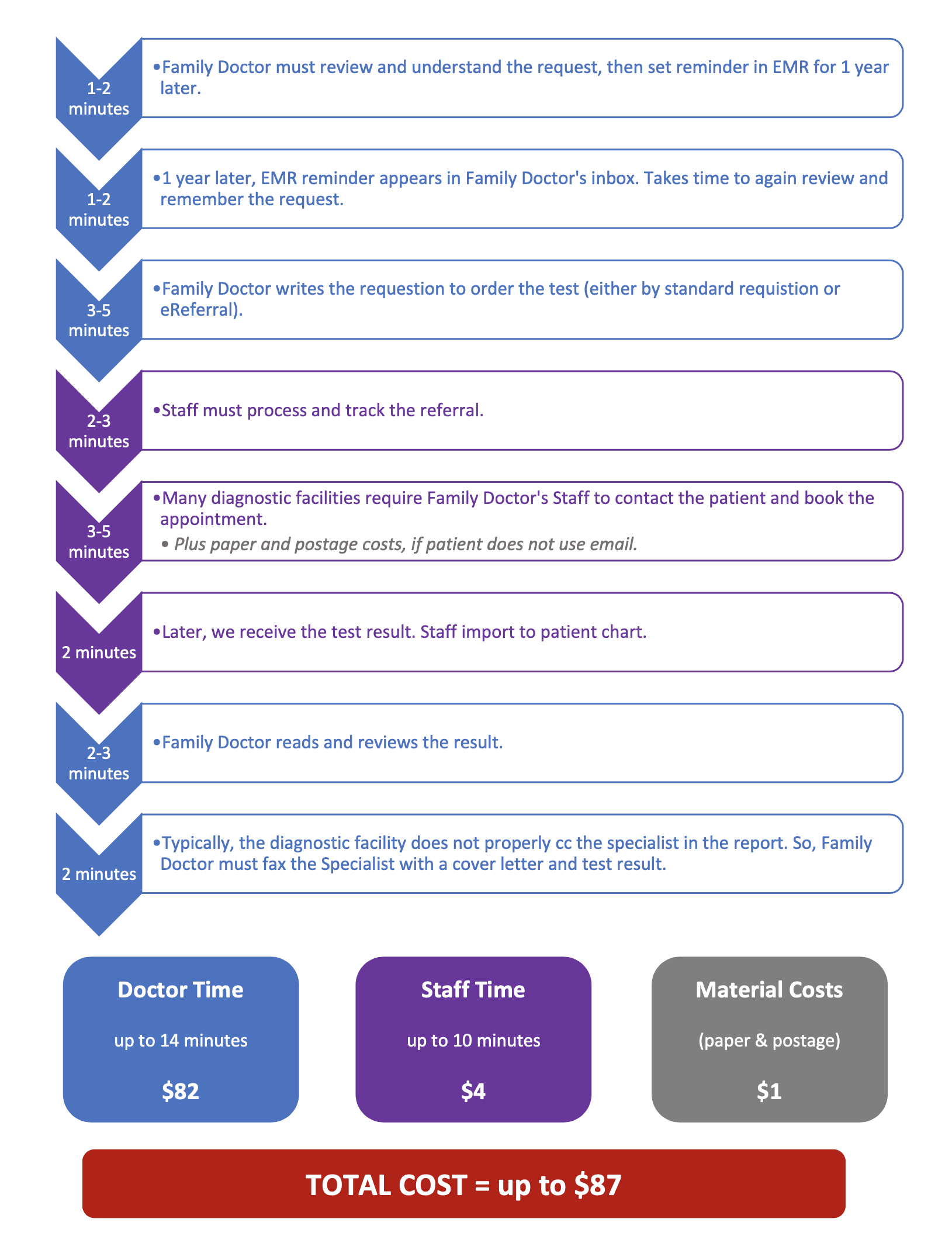
Regardless, let’s look at the costs when a patient is directed to the Family Doctor’s office for suture removal:
$10 may not seem like much. But it adds up when compounded multiple times each week. It certainly adds to the time and cost burden for Family Doctors.
Most importantly, though, all of the post-operative care for the first two weeks is included in the fee codes the surgeon bills to OHIP.
And again, the Family Doctor generates zero revenue here. The Family Doctor only incurs the costs because without seeing the patient, there are no OHIP codes the family doctor can bill here.
And paradoxically, it’s even worse when the Family Doctor needs to see the patient. When the nurse has a concern about wound healing, infection, or another post-operative complication, the nurse then has to find the Family Doctor, causing even more disruption and costs. (FHO Family Doctors only get to bill $3.56 or $5.52 in shadow-billings if called in to assess the post-operative patient, for what will surely amount to 10-20 minutes of work or more).
And if there are post-operative concerns, why again is the patient sitting in the Family Doctor’s office and not the Surgeon’s?
Specialists Direct Patients to see Family Doctors for Results
It is far too common for specialists to direct patients to follow up with Family Doctors for the results of tests or investigations they have themselves ordered.
For example, pathology results from a biopsy. Or imaging results. Or bloodwork results.
First of all, yet again, is it not in the patient’s best interest for the Specialist to be the one interpreting their own results? (Yet again, rhetorical).
But that aside, let’s again dive into to associated downloaded costs to the Family Doctor for requests like these:

Remember, all of this work is supposed to be included in the OHIP fee codes that the Specialist has already billed.
Yet, these costs are being downloaded to the Family Doctor.
This is not to mention that sometimes interpreting the results and context are outside the scope and expertise of the Family Doctor. So, many times, I have to redirect the patient back to contact the Specialist for the official final word. This makes the entire ordeal redundant and unnecessary to begin with.
It’s unacceptable.
What are the Alternatives?
The status quo is not sustainable for burnt out Family Medicine clinics.
So, here are two options:
- Specialists can comply with their obligations per the Schedule of Benefits. This may involve needing to hire additional support staff and invest in EMR technology, just as Family Doctors have been doing for decades for our own practice demands.
- Family Doctors, with our existing infrastructure, can act as administrative extensions for Specialists. But we will be sending an invoice to the Specialist for our services accordingly.
Remember, It’s a Two-Way Street
As stated at the beginning, this is a two-way street.
Thank you to all of our incredible Specialist colleagues who thoroughly follow our mutual patients.
(And it should be clarified that none of this applies to Emergency Physicians.)
Family Doctors must also fulfil our roles to our patients and to our Specialist colleagues. We have an obligation to provide quality, comprehensive, accurate referrals. We have a duty to be accessible to our patients for primary care. And we should be expected to be called out, if we are not doing so.
This article may be perceived as punitive or provocative by some. But in order for things to ever improve, we must first identify issues, raise awareness, and then have constructive discussions.
So let’s start. How can we improve each other’s work lives?
Respectfully,
Dr. Adam Stewart
February 12, 2023
